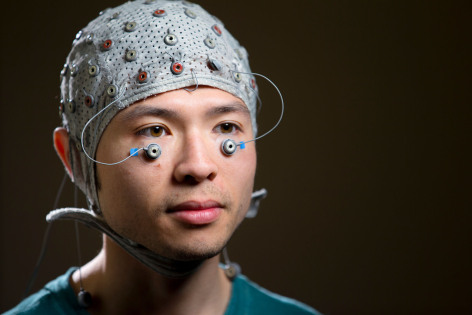
Data collected through EEG and with eye electrodes allowed researchers to measure brain activity and startle response. (Larger image) Photo by Christopher Gannon
AMES, Iowa – For millions of Americans who are obese and living with diabetes or prediabetes, feelings of sadness, anger and anxiety are often part of daily life.
A new Iowa State University study suggests those negative feelings may stem from problems regulating blood sugar levels that influence emotional response in the brain. The study found people with Type 2 diabetes and prediabetes were more likely to focus on and have a strong emotional response to threats and negative things, which affects quality of life and increases risk for depression. The research is published in the journal Psychosomatic Medicine.
Auriel Willette, an ISU assistant professor of food science and human nutrition; Tovah Wolf, lead author and a graduate student working with Willette on this project; and colleagues at the University of Wisconsin-Madison analyzed data on startle response, brain activity, cortisol levels and cognitive assessment. Data for the study came from Midlife in the U.S. (MIDUS), a national study of health and well-being.
Willette says gauging the startle response allowed researchers to measure central nervous system activity using tiny electrodes placed below the eye. Study participants viewed a series of negative, positive and neutral images intended to elicit an emotional response. The electrodes captured the rate of flinch or startle, a contraction we cannot control, associated with each image, he said.
“People with higher levels of insulin resistance were more startled by negative pictures. By extension, they may be more reactive to negative things in life,” Willette said. “It is one piece of evidence to suggest that these metabolic problems are related to issues with how we perceive and deal with things that stress all of us out.”
The researchers say the evidence is even more compelling when combined with the results of EEG tests recording activity when the brain is at rest. Study participants with prediabetes and Type 2 diabetes had more activity on the right side of the brain, which is associated with depression and negative emotions. If someone is predisposed to focusing on negative things, it may become a barrier for losing weight and reversing health issues, Wolf said.
People with prediabetes and diabetes also recorded lower cortisol levels – a potential indicator of chronic stress – and cognitive test scores, providing additional support for the findings.
Personal motivation
Understanding the effect of these biological factors is an important step in helping improve the quality of life for the one-third of Americans who are obese. Wolf, a registered dietitian, says her experience working with patients suffering from chronic diseases led her to this line of research. She often noticed differences in how patients responded to stress and wondered if that influenced their motivation to live a healthy life.
“For people with blood sugar problems, being more stressed and reactive can cause blood sugar to spike. If people with prediabetes and diabetes are trying to reverse or treat the disease, stressful events may hinder their goals,” Wolf said. “Frequent negative reactions to stressful events can lead to a lower quality of life and create a vicious cycle that makes it difficult to be healthy.”
Willette can relate. He struggled with weight, at one time weighing 260 pounds, which affected his day-to-day quality of life. Willette says the risk of cardiovascular disease and other chronic illnesses related to obesity is well known, but many people may not recognize how fluctuations in blood sugar can take a toll on them every day.
The researchers say additional work is needed to determine if the link between insulin resistance and emotional response is causal, and explore options for potential interventions. Vera Tsenkova, Carol D. Ryff and Richard Davidson, all with the University of Wisconsin-Madison, contributed to the research.

